Day 2 :
Keynote Forum
Samir Kumar-Singh
University of Antwerp, Belgium
Keynote: Immunosuppression and Infection
Time : 10:00-10:30

Biography:
Samir Kumar Singh is a Certified Medical Doctor with a Doctorate in Pathology and a Master’s degree in Laboratory Animals. He is a Full-Time Research Professor of Molecular Pathology at the Faculty of Medicine, University of Antwerp, Belgium and is affiliated to the Vaccine and Infectious Disease Institute, Belgium. He has published a well-cited body of work on molecular pathology of cancer and neurodegeneration involving patient studies and mouse modelling. He serves on several review and editorial boards and international consortia. Since 2012, his group is engaged in studying the pathomechanism of hospital acquired pneumonia especially ventilator-associated pneumonia (VAP) and has developed several authentic rat and mouse VAP as well as acute and chronic pneumonia models to study disease pathogenesis and for biomarker discovery as well as high-throughput in vitro screens for new antimicrobial targets.
Abstract:
While chemotherapeutic or immunosuppressive therapies have been considered as the therapeutic cornerstone for several clinical conditions such as cancer, autoimmune diseases and transplant rejection, these drugs are also known to increase the risk of infectious complications. While this is an important safety concern when prescribing immunosuppressive therapies to such patients, several human diseases show a natural immunosuppression that is also linked to a high risk of developing infectious complications. For instance, sepsis is one of the biggest causes of deaths in intensive care units and mortality is associated with both a hyperinflammatory cytokine-mediated disease phase and a protracted innate immune cell-driven immunosuppressive phase. Death associated with an immunosuppressive phase in sepsis, similar to HIV patients, is typically due to infectious complications with opportunistic pathogens. Similarly, in stroke patients, while a large proportion of immediate death is due to cerebral infarction and neurological complications, the most common post-stroke complication is that of infection, especially pneumonia, and which is equally responsible for the high morbidity and mortality observed in these patients. We have also recently shown that mechanical ventilation is linked with substantial innate immunosuppression and is likely linked to a high incidence of ventilator-associated pneumonia observed in these patients. This talk will address to mechanisms associated with some of these aetiologies and show how biomarker-directed research aiming to recognize early infections and preventive immune-based strategies could help to minimize the risk of infection and decrease morbidity and mortality in these aetiologies.
Keynote Forum
Tadashi Shimamoto
Hiroshima University, Japan
Keynote: Molecular characterization of carbapenemase-producing Gram-negative bacteria in Egypt
Time : 10:30-11:00

Biography:
Tadashi Shimamoto has completed his PhD from Okayama University, Japan and Post-doctoral studies from University of Medicine and Dentistry of New Jersey (now known as Rutgers University), Robert Wood Johnson Medical School, NJ, USA. He is a Professor of Graduate School of Biosphere Science, Hiroshima University, Japan. He has published more than 70 papers in reputed international journals
Abstract:
Twenty-six carbapenem-resistant Gram-negative bacterial isolates were recovered from clinical samples between April 2014 and September 2014 at Tanta University Teaching Hospital, Egypt. Carbapenemase production was detected phenotypically using Modified Hodge Test (MHT) and Carbapenem Inactivation Method (CIM) in 22 isolates. Molecular characterization identified the presence of thirteen NDM-1-producers (four Escherichia coli, two Klebsiella pneumoniae, and seven Providencia stuartii), two E. coli co-carrying NDM-5 and OXA-181, and seven VIM-producing Pseudomonas aeruginosa (three VIM-2, three VIM-24, and one VIM-28). For the other four isolates, no carbapenemase activity and no carbapenemase gene was detected, suggesting non-carbapenemase related resistance. The 16S rDNA methylase gene, rmtC was detected in twelve isolates (four E. coli, two K. pneumoniae, and six P. stuartii). The PCR mapping of the blaNDM gene showed that it was surrounded by a complete or truncated copy of insertion sequence ISAba125 and followed by a bleomycin resistance gene bleMBL, mediating resistance to bleomycin. ERIC-PCR analysis identified the presence of five clonally related P. stuartii isolates collected over a 1.5-month period. Each isolate, except one producing NDM-1 and the plasmid-mediated quinolone resistance gene qnrA, harbored NDM-1, and CMY β-lactamases and the 16S rDNA methylase gene, rmtC. To the best of our knowledge, this is the first report of an outbreak due to NDM-1-producing P. stuartii. Furthermore, ERIC-PCR analysis identified the presence of a clonal relationship between NDM-5-producing E. coli, VIM-2-producing P. aeruginosa, and VIM-24-producing P. aeruginosa. This work highlights the dissemination of different types of carbapenemases within a University Teaching Hospital in Egypt.
Keynote Forum
Siham M Mahgoub
Alzahra Hospital Dubai, UAE
Keynote: Aminoglycosides bladder irrigation for treatment of multidrug resistant organisms might be an option to treat complex cases of bacteriuria in the era of resistance and limited options
Time : 11:15-11:45

Biography:
Siham M Mahgoub, MD, is a board certified Infectious Diseases Consultant in the American Board of Internal Medicine. She is a Member of the Infectious Diseases Society of America (IDSA) & the Society for Health Care Epidemiology of America (SHEA). She received Residency Training at Beth Israel Medical Center (Albert Einstein School of Medicine), and Infectious Diseases fellowship in New York Medical College, New York. She has solid experience in Infectious Diseases Consultation in the USA including judicious use of antibiotic and is interested in antibiotic resistance.
Abstract:
Statement of the Problem: We are reporting a case of 51-year-old male with history of colectomy in 2013; followed in 2016 by laparotomy, bilateral ureteric stents, bladder repair complicated by vesicopouch fistula. He developed multiple Catheter related urinary tract infections with resistant organisms requiring multiple courses of antibiotics. He then had an extensive procedure: laparotomy, rectovesical fistula repair, revision of ileostomy, small bowel resection, urinary bladder repair and ureteric implants. He developed two episodes of catheter associated urinary tract infections (CAUTI) Extended-spectrum beta-lactamase (ESBL) and Carbapenem-resistant Enterobacteriaceae (CRE) requiring two hospitalizations and intravenous antibiotics. He was treated with Intravenous Amikacin but given his above history we decided to try Amikacin bladder irrigation which was done every other day for one week. The patient recovered after his last episode and he is now infection free for the past 3 months.
Materials & Methodology: One report showed that two cases were treated in 2009, followed for one year after treatment with daily intravesical gentamicin; the patients remained asymptomatic and infection free with negative urine cultures. Another report intravesicular Amikacin irrigation was used for the treatment and prophylaxis of a patient with spina bifida and neurogenic bladder; the patient was treated successfully but developed another episode two months later was retreated with intravenous antibiotics and intravesicular amikacin irrigation.
Findings: A retrospective study done on children treated with gentamicin bladder irrigation from 1999 -2004 found that bladder irrigation with aminoglycosides is safe, none of the patients had a detectable serum gentamicin. Out of 80 patients 21(26%) had recurrent UTI 5 (24%) had gentamicin resistance.
Conclusion & Significance: In the Era of antibiotic resistance and limited options for complex urologic cases aminoglycoside bladder irrigation is worth trying especially in patients who have no options but to have an indwelling catheter for prolonged period. Further studies to prove the efficacy of this modality of treatment are needed.
- Clinical Trials of Antibiotics | Modern Antibiotics for Various Diseases and Infections | Antibiotic Regulatory Affairs |Advances in Antibiotic Treatment | Antibiotics for Cancer | Antibiotics: In Pregnancy and Lactation | Antibiotic Prophylaxis | Antibiotics in Different Industries | Antibiotics for Emerging and Re-emerging diseases
Location: Conference Hall- Manzoni+Montenapoleone

Chair
Byungse Suh
Temple University, USA
Session Introduction
Fadya Al-Hamadani
Cardiff University, UK
Title: Antibiotics in care homes-a retrospective analysis of medicines administration records
Time : 11:45-12:05

Biography:
Fadya Hamadani has acquired her BSc in Pharmacy and MSc in Clinical Pharmacy from College of Pharmacy, Baghdad University (1992, 1998 respectively). She is Assistant Professor in Clinical Pharmacy and since that period, she has built a variety of experience in research, evaluation, teaching in higher education institutions and providing hospital training. Currently she is a full time PhD student at the School of Pharmacy and Pharmaceutical Sciences, Cardiff University. Her PhD project involves identification of issues around safe and effective administration and management of medicines in care homes. Her research interest includes the rational use of antibiotics in care homes.
Abstract:
Statement of the Problem: Residents of care homes are noted for the complexity of their care needs, multiple co-morbidities and the incidence of polypharmacy. This makes them particularly susceptible to medicines related harm. Antibiotic prescribing in care homes is particularly prevalent and their inappropriate administration risks the development of antimicrobial resistance. The aim of this present study was to identify the prevalence and types of prescribing and administration errors related to antibiotics in Care Homes.
Methodology & Theoretical Orientation: A retrospective study was conducted in 12 Care Homes in South Wales over an eight month period (Feb-Oct 2015). Anonymised real-time data was collected from an electronic medicines management system and the prevalence of antibiotic determined. The data was also analyzed for errors related to the prescribing and administration of antibiotics. The type and frequency of medication errors were recorded in excel and selected data was transferred into SPSS for further analysis.
Findings: A total of 142 (43.16%) residents received at least one antibiotic over the study period. The most commonly prescribed antibiotic was trimethoprim (24.6%). Some 9499 administrations were analyzed against pre-defined medication error categories with 2247 medication errors identified, 79.6% of residents were exposed to at least one error. The most frequent administration error type was duration error (44.5%) where the antibiotic was administered either for a period shorter or longer than the prescribed duration, followed by dose omissions errors (38.9%). The most common prescribing error type was similarly duration errors (74.3%).
Conclusion & Significance: This evaluation of the management of antibiotics in care homes in South Wales has revealed that the prevalence of antibiotic prescribing along with the incidence of administration and prescribing errors related to antibiotics is significant. This may result in antimicrobial resistance in a particularly vulnerable patient cohort.
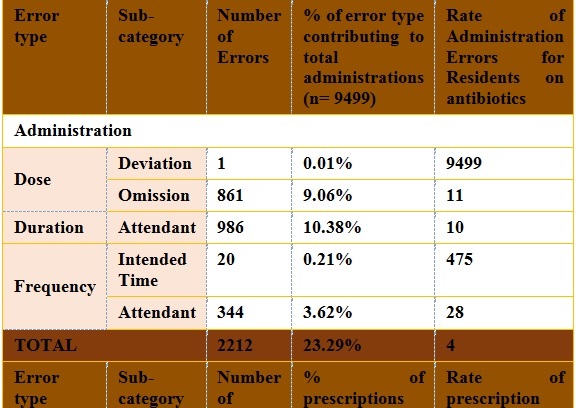
Table.1: Prescribing and administration errors for antibiotics in care homes
Yasir Al-Mehdi Edowik
Bangor University, UK
Title: A novel CTX-M14 related beta-lactamase renders E.coli sensitive to the antibiotic nitrofurantoin used to treat urinary tract infections
Time : 12:05-12:25

Biography:
Al-Mehdi Edowik Y is interested in Bacterial Antibiotic Resistance. After earning his Bachelor’s degree in Biomedical Science from Bangor University, he went through a one-year training period in the Public Health Wales Microbiology Department at Ysbyty Gwynedd Hospital, Bangor, where he gained experience in routine microbiology. Subsequently, he conducted an MSc (Master of Science) degree in Molecular Biology and Genetics at Bangor University. Currently he is undertaking a PhD in Molecular Microbiology at Bangor University. The research synopsis of his research is epidemiological gene carriage of ESBL-producing bacteria in UTI patients in North Wales.
Abstract:
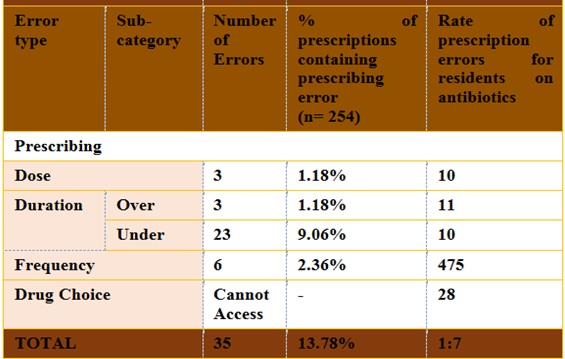
The antibiotic nitrofurantoin is indicated for the treatment of acute or recurrent lower urinary tract infections (UTI) which is caused by strains of Escherichia coli, Enterococci and Staphylococci, Citrobacter sp, Klebsiella sp or Enterobactersp. This study analyzed ESBL-producing bacteria isolated from 300 urine samples of UTI patients from three referral hospitals in North Wales, UK. Multiplex PCR amplification of β-lactamase genes of the blaCTX-M groups 1, 2, 9 and 8/25, followed by DNA sequencing revealed one new beta-lactamase gene which is closely related to CTXM‑14 at the protein levels. Recombinant expression of this new bla gene renders Escherichia coli highly resistant to nitrofurantoin. To characterize this new beta-lactamase, the enzyme was purified from the periplasmic space of E. coli or from the growth medium in a highly pure form, utilizing a C-terminal strep-tag. Isoelectric focusing and phostag electrophoresis revealed a high degree of phosphorylation and the presence of at least two distinct protein species. Since this new gene was isolated only from one of the three hospitals, it is quite possible that the new beta-lactamase is responsible for a local increase in nitrofurantoin resistance in UTI patients.
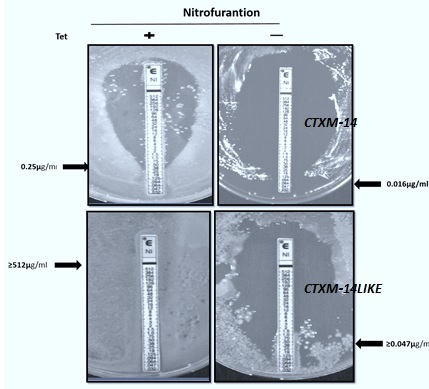
Figure 1: Induction of the novel CTX-M-14 related beta-lactamase renders cells resistant to Nitrofurantoin (E-Test Assay, + =induction of the recombinat enzyme; -= no induction.
Francisco Javier Alvarez Martinez
Miguel Hernandez University of Elche, Spain
Title: Antimicrobial capacity of plant extracts and pure polyphenolic compounds on intrahospital pathogenic species
Time : 12:25-12:45

Biography:
Álvarez-Martínez F J is a Molecular Biology PhD student at the Universidad Miguel Hernández of Elche. The main theme of his thesis is the identification of natural compounds with antimicrobial capacity to act as antibiotics or in conjunction with those already existing in the treatment of microbial diseases, especially those resistant to traditional drugs. To reach these objectives, computational approaches and in vitro studies using reference microbial strains are used in addition to clinical isolates collected at the General University Hospital of Alicante.
Abstract:
At present, the rise of multi-drug resistant microorganisms represents a serious threat to human health worldwide. The objective of the present work is the discovery of individual natural compounds or mixtures of them that have a remarkable antimicrobial capacity to be used as therapy against microorganisms resistant to antibiotics or as a complement to existing treatments. To carry out the tests of microbial susceptibility, we used ten natural agents with potential antimicrobial activity, including pure compounds and complex mixtures of them. The method chosen was disk-plate inhibition in Mueller Hinton (MH) medium, with positive results being those where the compounds produced an inhibition halo around the disc. The microbial species used in this study were Enterococcus faecalis, Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Enterobacter spp, Escherichia coli, Serratia marcescens, Salmonella spp, Pseudomonas aeruginosa, Stenotrophomonas maltophilia and Acinetobacter baumanii. All the strains were obtained from clinical isolates in the General University Hospital of Alicante. The most active formulations against microorganisms were two plant extracts and a pure compound, the major component of one of the previous extracts. The microbial species most affected by these natural agents were Staphylococcus aureus (between 62.1% and 72.4% of susceptible strains), Klebsiella pneumoniae (between 12.5% ​​and 25%), Enterobacter spp. 25%) and Stenotrophomonas maltophilia (between 37.5% and 62.5%). Three of the natural formulations tested exhibit a remarkable antimicrobial capacity against species of great clinical importance causing serious nosocomial infections. Given the results obtained, these naturally occurring formulations could be used in conjunction with known antibiotics to increase their efficacy and circumvent microbial resistance mechanisms. The next step is to characterize the effective concentrations of the natural formulations found in the present screening and possible synergy between them. The next tests will be performed using the p96 microdilution plate method.
Figure 1: Antimicrobial assay in p96 plate using ten different concentrations of natural agent against eight different isolates of Staphylococcus aureus.
Elisa Rampacci
University of Perugia, Italy
Title: In vitro cytotoxicity and efficacy against Rhodococcus equi of azithromycin plus rifampicin microparticle combinations
Time : 12:45- 13:05

Biography:
Elisa Rampacci received her degree in Veterinary Medicine from the University of Perugia. Currently, she is a PhD student in Health and Experimental Veterinary Sciences. She is making her experience in the field of in vitro and in vivo studies of antibiotic interactions, efficacy and toxicity of antimicrobial compounds. Particularly, her attention is focused on the treatment of zoonotic infectious diseases. Additionally, her interest is addressed towards pharmaceutical formulations potentially suited for not standard delivery routes associated with minor adverse effects.
Abstract:
Statement of the Problem: Rhodococcus equi is the main infectious agent of pneumonia in foals. This bacterium has recently gained attention as a zoonotic pathogen in immuno depressed people. Two-thirds of cases of R. equi infection in humans involved HIV-infected patients. However, 10%–15% of infections occur in immunocompetent hosts. In human medicine, rhodococcosis may be underdiagnosed because of frequent misidentiï¬cation for Mycobacterium tuberculosis. Combination treatment with two or more drugs is recommended both in equine and human infection in order to contrast the antibiotic resistance, especially including antibiotics with intracellular activity. The purpose of this study is to investigate the potential synergistic effect against R. equi of different azithromycin/rifampicin combinations formulated as dry powders and to assess their possible cytotoxicity.
Methodology & Theoretical Orientation: A broth microdilution test was performed to determine the minimum inhibitory concentration against R. equi of spray-dried azithromycin and rifampicin prepared independently and binary combinations of azithromycin and rifampicin developed as dry powders according to the ratios 1:1, 2:1 and 1:2 using mini spray-drying technology. The fractional inhibitory concentration indexes (FICIs) were calculated to describe drug interactions. Additionally, the minimum bactericidal concentration (MBC) was established. The cytotoxicity on BEAS-2B cells of azithromycin and rifampicin individually and in combination was assessed performing the MTT colorimetric assay.
Findings: FICIs calculation has confirmed the favorable additive effect of each antimicrobial combo. Moreover, MBC determination demonstrated the more powerful killing activity of combinations than single compounds. The MTT assay provided encouraging data about the combination application. Indeed, reduction of cellular viability below 50% was not observed neither at the highest concentration tested (100 µg/mL).
Conclusion & Significance: The additive interaction between azithromycin and rifampicin and the more powerful bactericidal activity of spray-dried combinations compared to single compounds may result in an improved therapeutic dosage and prevention of drug-resistant bacterial strains.
